Suboxone is highly recommended for addicts looking to recover from an opioid addiction. It has earned the nickname of “the box office drug”. This is likely due to the fact that it’s so popular that 1.55 billion US dollars worth of it was sold in 2013. This prescription medication dramatically reduces the severity of symptoms related to opiate addiction and withdrawal. The only negative aspect of Suboxone is that you can become addicted to it. Ironically, it’s possible to develop a secondary addiction to this treatment. Some drug abusers need addiction treatment from detox or rehabilitation centers when they’re trying to recover from an addiction to Suboxone. While this drug may be the better or two evils for those addicted to a dangerous drug like heroin, it needs to be used responsibly. Those who use this drug should use it as prescribed. They should take it on the recommended schedule and at the recommended dose. If they don’t, they may develop a tolerance to this drug. Eventually, they may find themselves falling into a similar pattern of addiction. An addiction to Suboxone requires its own course of treatment. A comprehensive treatment plan includes pharmacological and psychological treatment.
Suboxone Statistics
Suboxone is an incredibly popular medication used in substance abuse treatment. The numbers and the facts don’t lie. Here are some shocking statistics and facts about this drug:
- From 2002 to 2018, over 3 million Americans have taken Suboxone to treat opioid dependence.
- There were 30,135 buprenorphine-related emergency department visits in 2010. Buprenorphine is a crucial chemical component in Suboxone.
- 18,582 doctors in America were certified to prescribe Suboxone in 2010.
- 49% of recovering addicts who took Suboxone over the course of 12 weeks were able to reduce their use of painkillers.
- Doctors in America wrote over 9 million prescriptions for Suboxone in 2012.
This medication can treat an addiction to any opioids or opiates. It can be used to treat an addiction to illicit drugs, like heroin, and prescription drugs, like oxycodone. It’s versatile in nature, which makes it a highly recommended treatment option by many rehab centers. With that said, doctors are overprescribing this drug without letting patients fully understand the dangers of it.
What Is Suboxone?
Suboxone is an opioid medication used in Opiate Replacement Therapy (ORT). It is safer than methadone, and is used for the same purpose. It’s considered a highly effective treatment option for addiction and was administered to 3 million patients in 2012. Suboxone is a mixture of buprenorphine and naloxone. 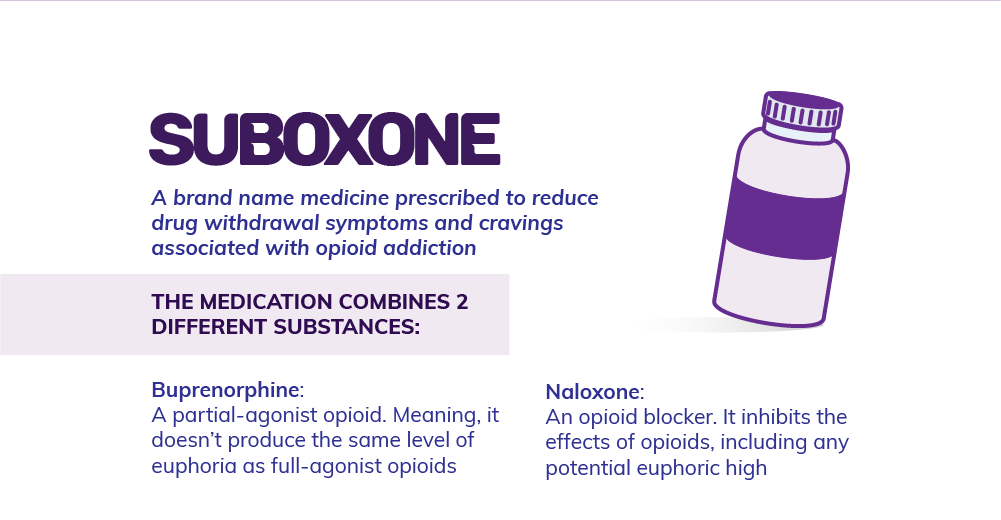
How the Medical Field Mismanaged Suboxone
Suboxone abuse and misuse comes from doctors prescribing Suboxone as a maintenance drug in the same way that methadone was prescribed for years. This has led some patients to maintain their Suboxone use for years at a time. This is where the trouble starts. These same patients, who are doing their best to overcome their addictions to narcotics, are given another drug that is just as addictive. Basically, all doctors were doing was substituting an illegal drug for a similar drug that’s legalized. The addiction is the same. Patients still have a physical dependence on an opioid-type drug. Years later, people are discovering that they can’t stop taking Suboxone. They have to continue taking doses of the drug to prevent opiate withdrawal symptoms. Some people are even using heroin as a replacement if they can’t afford to get their prescriptions any longer. Doctors have misled patients into believing that this drug is a cure for their addictions. The medical system let people down and caused Suboxone to be overprescribed. This may also be due to the fact that doctors don’t need to have any specific training on addiction to prescribe this medication. This has led to a grave mismanagement of Suboxone use. Although this prescription drug is effective in treating opioid addiction, it’s caused another problem of its own. Perhaps, if doctors had known about the long-term effects of the long-term use of this drug, they would have thought differently about it.
What Does Suboxone Do to Help You Recover
Your addiction can be managed properly with the help of Suboxone. The benefit of Suboxone is its ability to aid you in recovery. The emotional and physical withdrawal symptoms are overwhelming. 
- Pain relief
- Calmness and relaxation
- Reduced stress levels
In general, they won’t experience any of the withdrawal symptoms commonly associated with opiate abuse. This is what makes Suboxone so special. It’s important to note that Suboxone is not the only drug capable of accomplishing this. Methadone and Vivitrol are two other alternatives capable of producing similar effects. Each of these other drugs also has its own unique features and advantages. The ingredients in Suboxone are buprenorphine and naloxone. Buprenorphine sits in opiate receptors and blocks them, so opiates cannot attach. This ensures that you don’t suffer from withdrawal symptoms. It binds tightly to receptors, allowing for an even level of neurochemical production all day. So, how does this compare to short-acting compounds? An example of a short-acting agonist is heroin. It wears off fairly quickly. This forces you to take increasingly larger doses to get the euphoric effect you desire. Naloxone, which is the second chemical compound in this medication, is a pure opioid antagonist. An agonist excites the opioid receptor while an antagonist shuts it down. As a result, naloxone blocks your ability to feel the effects of opiates. Naloxone also reverses the effects of opioid agonists that are currently in your system. This allows the body to slowly become less stimulated by its opioid receptors. There is a risk of shutting off opioid receptors in the body. Abrupt cessation can set off withdrawal symptoms that involve the mind and body. You may become highly irritable with fast “highs” and “lows” while dealing with nausea, muscle cramping, diarrhea or vomiting. The combination of buprenorphine and naloxone in Suboxone gives you a smoother transition from strong narcotics. Suboxone starts working the day you begin using it. You will begin to feel normal again and not experience physical symptoms like aching pain, vomiting, and diarrhea. You can eat, sleep, and go to work. Life can begin to get back to normal. This is the upside of Suboxone when it’s administered correctly.
Suboxone is a Replacement for Opioids
Suboxone for opioid addiction is like insulin for a diabetic. The medication regulates your brain chemistry when you use it everyday. It allows you to feel well in spite of the fact you’ve stopped using harmful opiates. It doesn’t actually fix the initial problem, and it doesn’t mean other treatment options shouldn’t be considered. To really fix the fundamental components of this issue, you need to focus on other ways to regulate your brain chemistry. This helps the medication work optimally and you can begin to decrease the Suboxone dosage to the lowest amount. If you’re truly motivated to recover, it will be important to taper off Suboxone and live life in a way that makes relapse less likely. This might not be so easy to do on your own so seeking guidance from an addiction treatment center can increase chances of a full recovery. Pair Suboxone treatment with other types of treatments for a better shot at recovery. Your treatment plan should not only include medical detox. It should also include other treatments, like:
- One-on-one counseling and therapy
- Group counseling and therapy
- Family programs
- Behavioral therapy, like Cognitive Behavioral Therapy (CBT)
- Holistic treatment options
- Classes that teach independent life skills
- Trauma treatment
You can get the treatment you need from both inpatient and outpatient care. Inpatient treatment programs are a bit more rigid, but they offer the highest level of care possible. Patients receive around-the-clock supervision and care. Outpatient care, on the other hand, is a bit more flexible. Both options, when paired with Suboxone treatment, can help opiate abusers get their life back on the right track.
Suboxone Doesn’t Resolve the Reason You Became an Addict
Suboxone helps with physical symptoms of dependence, but beating addiction takes more work than that. You also need to heal from the mental or emotional issues that led you to addiction in the first place. This often means that you’ll need a safe place where you can speak with other people or get one-on-one therapy. It’s important to determine what are the core emotional issues that led you to make the choices you have. Figuring out your reasons for abusing drugs can be a painful journey. You will need to dive deep into your psyche to find the answers. Although the experience may not be pleasant, it’s necessary. These reasons are the answers to how you can stay clean forever. Suboxone is not designed for long-term use. It is just a small part of the whole picture when it comes to recovery from addiction. Solely relying on it will just create a new addiction. Suboxone works well so it’s possible you may believe you have kicked your addiction. However, if you continue to use it after completing detox, you may develop a physical and chemical dependence to it. You will experience withdrawal symptoms when you try to stop taking it. Common withdrawal symptoms include anxiety, difficulties sleeping and a sense of dread. These small nuances can make it challenging to go about your daily life. It may even make it difficult to enjoy life.
Suboxone Can Lead to an Opioid Overdose
You may experience Suboxone withdrawal symptoms in the following two situations:
- You try to decrease your dose of the medication too quickly.
- You quit and go cold turkey.
If you don’t take Suboxone as prescribed, there’s a good chance that you’ll relapse. 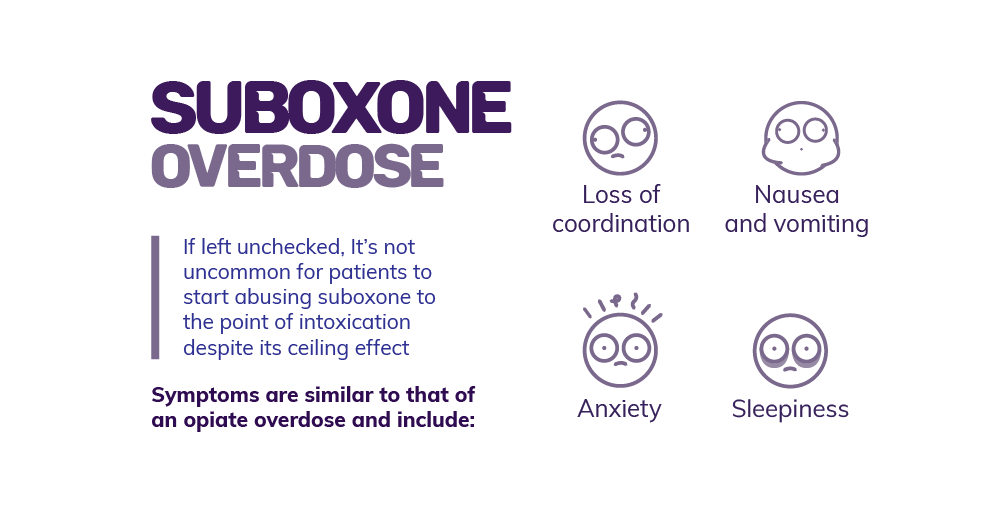
- Abdominal pain
- Anxiety, irritability and intense mood swings
- Difficulties concentrating or remembering things
- Extreme exhaustion and sleepiness
- Loss of coordination
- Nausea and vomiting
- Respiratory depression and even failure
- Seizures and tremors
- Slowed heartbeat
In extreme cases, an overdose can even lead to coma or death. A Suboxone overdose is no laughing matter and should be taken very seriously. If you or someone you know has overdosed on Suboxone, the one thing that you have to do is call 9-1-1 immediately. Only emergency medical attention can help an overdose victim survive the overdose. Provide the emergency responder with as much information as possible. This includes information like:
- The dose taken
- The frequency and length of the abuse
- Whether other substances were taken at the same time
- Whether the overdose victim struggles with a co-occurring disorder
- The severity and type of overdose symptoms exhibited
If naloxone is available, administer it as soon as possible. Naloxone is an opioid-reversing medication that comes in two forms: an injection or a nasal spray. Both method of administration will start to take effect within 5 to 30 minutes. If it doesn’t, a second dose needs to be administered. It’s important to note that naloxone isn’t a cure although it may temporarily stop an overdose. Naloxone has a fairly short half-life of about 3 hours. Once it wears off, the overdose victim can still continue to experience symptoms of an overdose.
Suboxone Withdrawal Symptoms
Keep in mind that it’s possible to experience Suboxone withdrawal symptoms as well. This happens if you try to quit cold turkey. The withdrawal symptoms are similar to withdrawal symptoms for heroin or methadone. Here are some of the side effects of Suboxone withdrawal that you may experience. These symptoms are much more likely to emerge if you don’t taper off the medication little by little. Common withdrawal symptoms include:
- Nausea and vomiting
- Aching muscles and joints
- Difficulties sleep
- Drowsiness
- Stomach problems like indigestion
- Negative mood fluctuations like anxiety, depression, or irritability
- Uncomfortable feelings and intense cravings
- Fever or chills
- Uncontrollable sweating
- Headaches or migraines
- An inability to think clearly
Symptoms of Suboxone withdrawal can vary in severity and intensity. The timeline can also vary in duration. A lot of different factors come into play. It all depends on how long the individual are taking the medication for, as well as the dose that they were taking. 
Timeline of Suboxone Withdrawal
The length of the withdrawal timeline will depend on the amount of time you were on Suboxone. Usually, the physical withdrawal symptoms will last for four weeks, but psychological dependence on the medication may last for an even longer time. 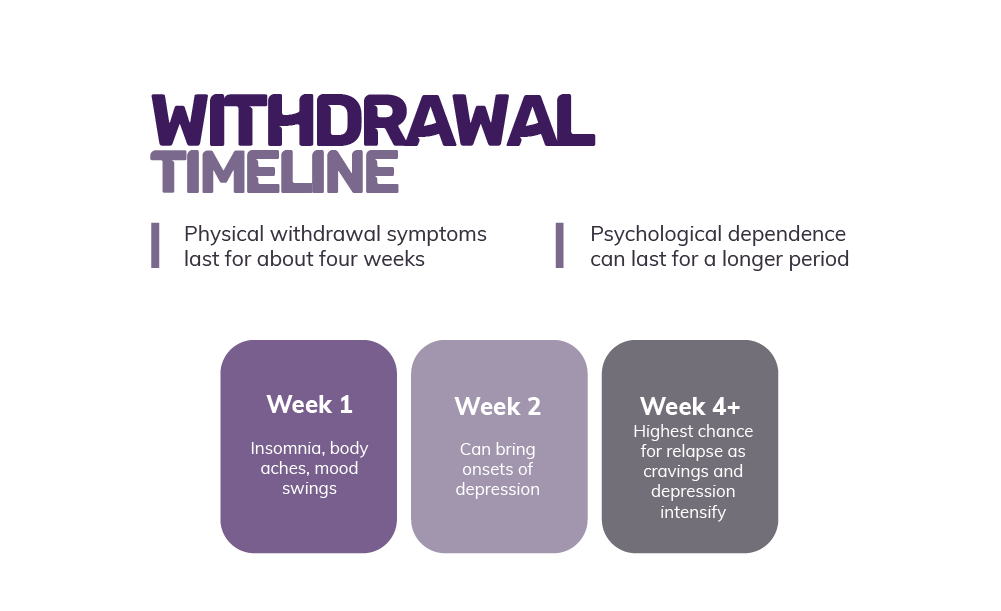
- 0 to 72 hours: This is when the physical symptoms start to appear. They will slowly start to worsen and will usually peak by 72 hours.
- 73 hours to one week: Drug abusers will continue to experience body aches and pains, insomnia and mood swings. Most of the physical symptoms will start to subside by this point.
- 2 weeks forward: Patients start to feel depressed, antsy and suicidal. This is when they need social support the most. This is when drug abusers will benefit from Narcotics Anonymous (NA) meetings the most.
- 1 month: Physical symptoms will have usually all subsided. All that’s left is the psychological symptoms, like cravings and depression. These symptoms are difficult to treat.
As mentioned above, patients are not likely to experience this exact timeline. The variation in the length of the timeline will depend on each patient, as well as their situation. As symptoms of Suboxone withdrawal can be very unpleasant, most rehab centers will try to help patients avoid it entirely. This is possible for those who slowly taper off of the drug. Even if the symptoms are not avoided entirely, they can be less intense.
How to Taper Off Suboxone
Can you get off Suboxone and experience minimal withdrawal symptoms? The answer is yes if you have the right taper schedule. The taper schedule for Suboxone will vary depending on each patient. It will also depend on the opinions of the addiction specialists at the drug rehab center. Many studies have looked at the best taper schedule for this medication. Clinical studies have found that pairing Suboxone treatment and behavioral therapy for30 days can help many opioid users break free from addiction. This treatment plan will, then, need to be followed by a 14-day taper schedule. 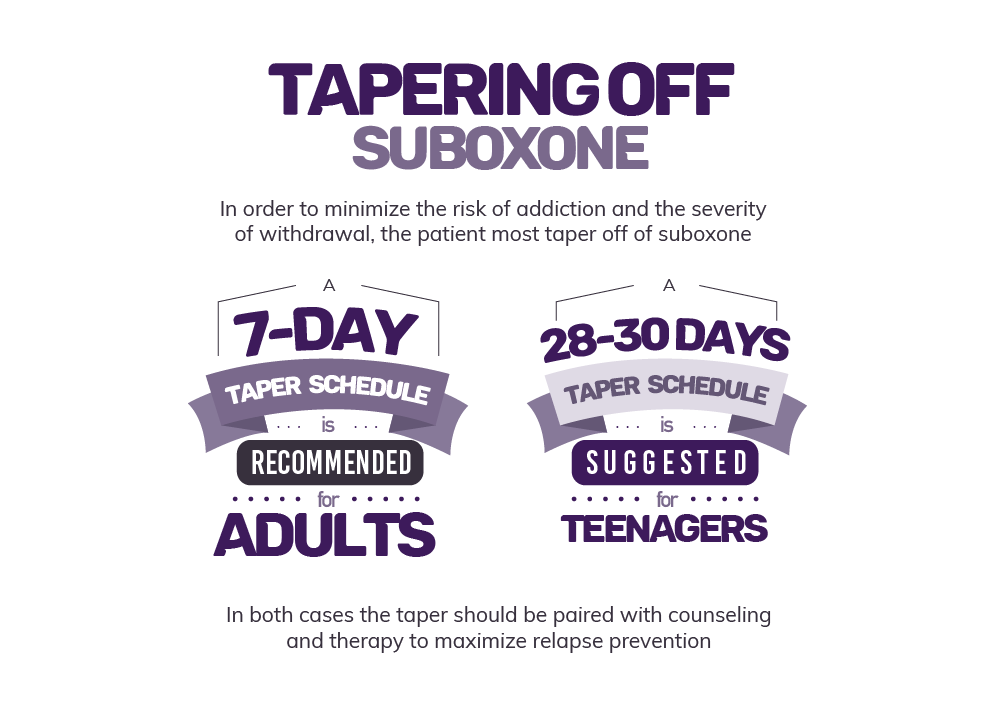
- Pace the taper. There’s no rush to get to the finish line. If you ever feel that you’re tapering too quickly, you can always slow the taper schedule down. Just speak with a professional.
- End the taper at the lowest dose possible. By doing so, you’re less likely to experience any withdrawal symptoms when you eventually come off of the drug.
- Pause the taper and go back to the last dose if you experience intense symptoms. Everyone’s body works differently. Just because someone can taper off Suboxone quickly, it doesn’t mean that you can. Pause the taper and go back to the last dose for a more comfortable recovery.
- Enjoy mid-taper breaks. Speak to an addiction specialist if you ever feel like the taper schedule is too overwhelming. You may need a break.
- Take the dose in the morning. Many experts believe that patients who take the dose in the morning will enjoy the most out of the medication. They are less likely to experience withdrawal symptoms during the day.
- Exercise and take part in therapy. Mindfulness, therapy and holistic treatments can take your mind off of the withdrawal timeline and process. It will help speed up your recovery, and may even help you build character.
By following the tips and tricks above, many patients agree that getting off Suboxone was easy. They didn’t experience any intense withdrawal symptoms. If they did experience symptoms, the symptoms were mild and not too unbearable.
Use Suboxone as Prescribed to Avoid All the Negatives
If you’re struggling with an opioid or opiate addiction, you should still consider using Suboxone to help you break free from your addiction. Suboxone is one of the safest and most effective treatment options out there. It’s also fairly affordable and comes with minimal side effects. This makes it an incredibly popular medication among recovering drug addicts. The only thing you need to be careful with is making sure that you adhere to the prescription schedule and dose. Do not deviate from the treatment plan provided to you by your doctor. You can develop a secondary addiction if you do or if you intentionally misuse or abuse this drug. Since there are some risks involved with using Suboxone, the best thing that you can do for yourself is to get professional help. Here, at Denver Women’s Recovery, we have the means to help you conquer an addiction. We also know how to help you use Suboxone in the right way, so that you don’t end up with another addiction. If you’re interested in our treatment programs, don’t hesitate to contact us. Our addiction professionals can even help you determine whether this addiction medication is covered under your insurance plan. We’ve got you covered, so you can focus solely on your recovery.